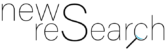
Approximately one fifth (22 percent) of COVID-19 patients treated in hospitals died (Figure 1). The mortality rate for men (25 percent) was 6 percentage points higher than that for women (19 percent). Mortality among older patients was very high, irrespective of gender: 27 percent of patients aged 70 to 79 died, with the number rising to 38 percent for patients over 80 years.
High mortality rate among ventilated patients
Slightly more than half of all patients requiring mechanical ventilation died (53 percent). The highest rates were among patients aged 70 to 79 (63 percent) and patients aged over 80 (72 percent). The mortality rate for ventilated patients treated with dialysis due to kidney failure during hospitalization (27 percent of all ventilated patients) was also very high at 73 percent. The mortality rates for men and women requiring ventilation were similar. The number of patients not receiving ventilation who died was significantly lower, but still reached 16 percent. Here again, there was a correlation between age and mortality. “These high mortality rates clearly show that a relatively high number of patients with a very serious course of disease were treated in hospitals. Such serious course of diseases mainly affect older people and people whose health is already compromised, but also occur in younger patients,” says Jürgen Klauber, director of WIdO. “Even though infection rates in Germany are currently low, we should continue to take all necessary precautionary measures to ensure that the risk of infection remains as low as possible.”
Almost twice as many men as women with COVID-19 receive ventilation
The data for COVID-19 patients with and without mechanical ventilation were analyzed separately. Of the 10,021 hospitalized COVID-19 patients, 1,727 received mechanical ventilation. Just over three quarters of ventilated patients were treated with invasive ventilation. The average age of patients was 68 – in both the ventilated and the non-ventilated group. The proportion of patients receiving ventilation according to age group were as follows (Figure 2): Among those aged 60 to 69 and those aged 70 to 79, it was 24 percent and 25 percent, respectively, it was 15 percent of those aged 18 to 59 and 12 percent for patients aged 80 and over. “Although the proportion of older patients receiving ventilation is relatively low, we can assume that in Germany all patients requiring this treatment will have received it. This is due to the fact that during the entire pandemic, there have always been enough intensive care beds available across Germany and fortunately the capacity of the intensive care units was never fully utilized,” says Christian Karagiannidis, speaker of the lung and respiratory failure section of DIVI and head of the ECMO center at the Cologne-Merheim lung clinic. “International comparisons are difficult due to the different samples used in studies. There is, however, evidence to suggest that less old people with COVID-19 have received ventilation in other countries – presumably due to the capacities available.”
An examination of data by gender also produces interesting results: Although the proportion of men receiving ventilation (22 percent) was almost twice as high as that of women (12 percent), mortality rates were similar. “The administrative claims data provides us with no explanation for this imbalance and further research is required,” says Karagiannidis.
Ventilated patients are more likely to have comorbidities
COVID-19 patients treated in hospitals often suffer from a range of comorbidities (Figure 3). The number of patients with comorbidities was considerably higher among those who received ventilation than among those who did not. For example, 24 percent of patients not receiving ventilation had cardiac arrhythmias as opposed to 43 percent among those who did receive ventilation. Diabetes was present in 26 percent of patients without ventilation but in 39 percent for ventilated patients.
Half of ventilated patients received ventilation for more than 10 days
The average length of hospital stay for COVID-19 patients was 14 days. It was considerably shorter at 12 days for patients without ventilation than for patients with ventilation (25 days). Duration of ventilation was on average 14 days with a median period of 10 days (Figure 4). 23 percent of patients required mechanical ventilation for more than 21 days. “Our analyses provide useful data for forecasts regarding hospital and ventilation capacities. We observe that on average 240 days of ventilation are required for every 100 hospitalized patients. These are important numbers to prepare for a second wave of the pandemic. However, we do not anticipate any problems with normal hospital beds, even with high infection rates,” says Reinhard Busse, professor of health care management at TU Berlin.
First national study for Germany based on extensive and high-quality data
The study analyzed 10,021 patients with confirmed cases of COVID-19 who were admitted to 920 German hospitals between 26 February and 19 April 2020 and have already been discharged or died in hospital. It is the most extensive study of COVID-19 patients treated in German hospitals to date. The underlying sample of AOK-insured persons corresponds to about one third of the total population and is representative in age and gender. Many of the internationally published studies using large databases include patients who are still in hospital. This means that for these studies length of hospital stay and duration of ventilation as well as mortality rates cannot yet be precisely determined.
Link to the publication:
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30316-7/fulltext
WIdO Wissenschaftliches Institut der AOK
Rosenthaler Straße 31
10178 Berlin
Telefon: +49 (30) 34646-2393
Telefax: +49 (30) 34646-2144
http://www.wido.de
Press office
Telefon: +49 (30) 34646-2309
E-Mail: presse@wido.bv.aok.de
Press office
Telefon: +49 (89) 2306960-69
E-Mail: presse@divi.de
Office of Communication, Events and Alumni
Telefon: +49 (30) 314-27879
E-Mail: pressestelle@tu-berlin.de
![]()